Hip Replacements
 Whether you have just begun exploring treatment options or have already decided with your orthopaedic surgeon to undergo hip replacement surgery, this information sheet will help you understand the benefits and limitations of this orthopaedic treatment. You’ll learn how a normal hip works and the causes of hip pain, what to expect from hip replacement surgery and what exercises and activities will help restore your mobility and strength and enable you to return to everyday activities.
Whether you have just begun exploring treatment options or have already decided with your orthopaedic surgeon to undergo hip replacement surgery, this information sheet will help you understand the benefits and limitations of this orthopaedic treatment. You’ll learn how a normal hip works and the causes of hip pain, what to expect from hip replacement surgery and what exercises and activities will help restore your mobility and strength and enable you to return to everyday activities.
If your hip has been damaged by arthritis, a fracture or other conditions, common activities such as walking or getting in and out of a chair may be painful and difficult. You may even feel uncomfortable while resting.
If medications, changes in your everyday activities, and the use of walking aids such as a cane are not helpful, you may want to consider hip replacement surgery. By replacing your diseased hip joint with an artificial joint, hip replacement surgery can relieve your pain and help you get back to enjoying normal, everyday activities.
First performed in 1960, hip replacement surgery is one of the most important surgical advances of this century. Since then, improvements in joint replacement surgical techniques and technology have greatly increased the effectiveness of this surgery. Today, more than 75,000 total hip replacements are performed each year in the UK. Similar surgical procedures are performed on other joints, including the knee, shoulder, and elbow.
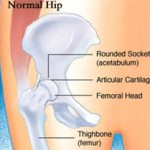
 The hip is one of your body’s largest weight-bearing joints. It consists of two main parts: a ball (femoral head) at the top of your thighbone (femur) that fits into a rounded socket (acetabulum) in your pelvis. Bands of tissue called ligaments connect the ball to the socket and provide stability to the joint.
The hip is one of your body’s largest weight-bearing joints. It consists of two main parts: a ball (femoral head) at the top of your thighbone (femur) that fits into a rounded socket (acetabulum) in your pelvis. Bands of tissue called ligaments connect the ball to the socket and provide stability to the joint.The bone surfaces of your ball and socket have a smooth durable cover of articular cartilage that cushions the ends of the bones and enables them to move easily.
All remaining surfaces of the hip joint are covered by a thin, smooth tissue called synovial membrane. In a healthy hip, this membrane makes a small amount of fluid that lubricates and almost eliminates friction in your hip joint.
Normally, all of these parts of your hip work in harmony, allowing you to move easily and without pain.
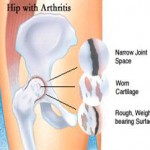
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and traumatic arthritis are the most common forms of this disease.
Osteoarthritis usually occurs after age 50 and often in an individual with a family history of arthritis. In this form of the disease, the articular cartilage cushioning the bones of the hip wears away. The bones then rub against each other, causing hip pain and stiffness.
Rheumatoid Arthritis is a disease in which the synovial membrane becomes inflamed, produces too much synovial fluid, and damages the articular cartilage, leading to pain and stiffness.
Traumatic Arthritis can follow a serious hip injury or fracture. A hip fracture can cause a condition known as avascular necrosis. The articular cartilage becomes damaged and, over time, causes hip pain and stiffness.
The decision whether to have hip replacement surgery should be a cooperative one between you, your family, your GP, and your orthopaedic surgeon. The process of making this decision typically begins with a referral by your doctor to an orthopaedic surgeon for an initial evaluation.
While most patients who undergo hip replacement surgery are age 60 to 80, orthopaedic surgeons evaluate patients individually. Recommendations for surgery are based on the extent of your pain, disability, and general health status, not solely on age or x-ray appearance.
You may benefit from hip replacement surgery if:
- Hip pain limits your everyday activities such as walking, bending.
- Hip pain continues while resting, either day or night
- Stiffness in a hip limits your ability to move or lift your leg.
- You have little pain relief from anti-inflammatory drugs.
- You have harmful or unpleasant side effects from your hip medications.
- Other treatments such as physical therapy don’t relieve hip pain.
Your orthopaedic surgeon will review the results of your evaluation with you and discuss whether hip replacement surgery is the best method to relieve your pain and improve your mobility. Other treatment options such as medications, physical therapy, or other types of surgery also may be considered.
Your orthopaedic surgeon will explain the potential risks and complications of hip replacement surgery, including those related to the surgery itself, and those that can occur over time after your surgery.
- A medical history, in which your orthopaedic surgeon gathers information about your general health and asks questions about the extent of your hip pain and how it affects your ability to perform every day activities.
- A physical examination to assess your hip’s mobility, strength, and alignment.
- X-rays to determine the extent of damage or deformity in your hip.
- Occasionally, blood tests, or other tests such as an MRI (Magnetic Resonance Imaging) or a bone scan may be needed to determine the condition of the bone and soft tissues of your hip.
An important factor in deciding whether to have hip replacement surgery is understanding what the procedure can and can’t do.
The vast majority of individuals who undergo hip replacement surgery experience a dramatic reduction of hip pain and a significant improvement in their ability to perform the common activities of daily living. However, hip replacement surgery will not enable you to do more than you could before your hip problem developed.
Following surgery, there are relatively few limitations in terms of sports and exercise and the aim of surgery is to return patients to activities they enjoy.
Even with normal use and activities, an artificial joint (prosthesis) develops some wear over time so the younger someone is at the time of their first hip replacement, the greater the chance that some of re-do may be necessary. Currently, however, with modern materials such as a ceramic on ceramic articulation, we are not seeing any signs of wear or loosening even after 25 years.
Medical Evaluation: If you decide to have hip replacement surgery, you may need a review of any concurrent medical illnesses. This is needed to assess your health and find conditions that could interfere with your surgery or recovery.
Tests: Several tests, such as blood samples, a cardiogram, chest X-rays, and urine sample may be needed to help plan your surgery.
Preparing Your Skin Your skin: should not have any infections or irritations before surgery. If either are present, contact your orthopaedic surgeon for a program to improve your skin before your surgery.
Medications: Tell your orthopaedic surgeon about the medications you are taking. Your orthopaedic surgeon or your GP will advise you which medications you should stop or can continue taking before surgery.
Weight Loss: If you are overweight, your doctor may ask you to lose some weight before surgery to minimize the stress on your new hip.
Dental Evaluation: Although infections after hip replacement are not common, an infection can occur if bacteria enter your bloodstream. Since bacteria can enter the bloodstream during dental procedures, treatment of significant dental diseases (including tooth extractions and periodontal work) should be considered before your hip replacement surgery.
Urinary Evaluation: A urological evaluation before surgery should be considered by individuals with a history of recent or frequent urinary infections.
Social Planning: Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry. If you live alone, your surgeon’s office, a social worker, or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at your home. A short stay in an extended care facility during your recovery after surgery also may be arranged.
Here are some items and home modifications that will make your return home easier during your recovery.
- Securely fastened safety bars or handrails in your shower or bath.
- Secure handrails along all stairways.
- A stable chair for your early recovery with a firm seat cushion that allows your knees to remain lower than your hips. a firm back, and two arms.
- A raised toilet seat.
- A stable shower bench or chair for bathing.
- A long-handled sponge and shower hose.
- A dressing stick, a sock aid, and a long-handled shoe horn for putting on and taking off shoes and socks without excessively bending your new hip.
- A reacher that will allow you to grab objects without excessive bending of your hips.
- Firm pillows to sit on that keep your knees lower than your hips for your chairs, sofas, and car.
- Removal of all loose carpets and electrical cords from the areas where you walk in your home.
You will most likely be admitted to the hospital on the day of your surgery. After admission, you will be evaluated by an anaesthetist. The most common types of anaesthesia for hip replacement surgery are general anesthesia (which puts you to sleep throughout the procedure) or spinal anesthesia (which allows you to be awake but anesthetises your body from the waist down). The anaesthetist will discuss these choices with you and help you decide which type of anaesthesia is best for you.
The surgical procedure takes one to two hours. Your orthopaedic surgeon will remove the damaged cartilage and bone, then position new metal and plastic joint surfaces to restore the alignment and function of your hip.
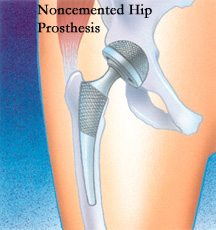
Many different types of designs and materials are currently used in artificial hip joints. All of them consist of two basic components: the ball component (made of a highly polished strong metal) and the socket component (a durable plastic cup which may have an outer metal shell).
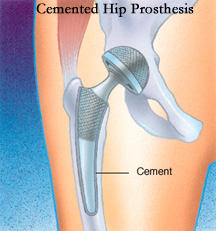 A special surgical cement may be used to fill the gap between the prosthesis and remaining natural bone to secure the artificial joint.
A special surgical cement may be used to fill the gap between the prosthesis and remaining natural bone to secure the artificial joint.
A noncemented prosthesis has also been developed which is used most often in younger, more active patients. The prosthesis may be coated with textured metal or a special bone-like substance which allows bone to grow into the prosthesis.
Your orthopaedic surgeon will choose the type of prothesis that best meets your needs.
After surgery, you will be moved to the recovery room where you will remain for one to two hours while the recovery from anesthesia is monitored. After you awaken fully, you will be taken to your hospital room.
You will stay in the hospital for a few days. After surgery, you will feel pain in your hip. Pain medication will be given to make you as comfortable as possible.
To avoid lung congestion after surgery, you will be asked to breathe deeply and cough frequently.
Walking and light activity are important to your recovery and will begin on the day or the day after your surgery. Most hip replacement patients begin standing and walking with the help of a walking support and a physical therapist the day after surgery. The physical therapist will teach you specific exercises to strengthen your hip and restore movement for walking and other normal daily activities.
The complication rate following hip replacement surgery is low. Serious complications, such as joint infection, occur in less than 2 percent of patients. Major medical complications, such as heart attack or stroke, occur even less frequently. However, chronic illnesses may increase the potential for complications. Although uncommon, when these complications occur they can prolong or limit your full recovery.
Blood clots in the leg veins or pelvis are the most common complication of hip replacement surgery. Your orthopaedic surgeon may prescribe one or more measures to prevent blood clots from forming in your leg veins, such as special support hose, inflatable leg coverings, and blood thinners.
Complications related to the hip replacement procedure:
Infection: Fortunately this is rare occurring in a little less than 1% of cases. If it occurs, however, it can result in an extensive period of treatment to remove the infection. This may involve removing the implants as it is difficult to treat infection while the implants remain in place and a temporary device maybe inserted to function as the hip until the infection has been treated. Usually this will require 6 weeks to 3 months of antibiotic therapy.
Dislocation: This happens if the new ball is forced out of the socket and can occur with certain positions of the hip. This is most common in the early weeks after hip surgery as the tissues around the hip are healing. The risk is in the region of 1%. If it happens the hip can usually be put back into place without open surgery
Nerve injury and bleeding: There are important nerves and blood vessels around the hip and approaches are designed to take care and look after these. There can be times when a nerve or blood vessel could be stretched or injured and this could result in some loss of function in the leg. Often after a nerve injury there will be a gradual recovery but this may not be complete. This is an unusual complication but may occur in 0.5-1% of cases.
Leg length change: There may be a leg length difference after hip replacement surgery and mostly this might be a few millimetres and not noticeable. Occasionally it could be more. The aim of the surgery is to keep leg lengths equal but it is also important that the hip is stable with a low chance of dislocation and the joint relies on the correct tension in the soft tissues to keep it stable. Every effort is made to optimise leg lengths by planning before surgery and taking a number of measurements during surgery.
Fracture: During surgery it is possible that when the implants are being put in the bone or the bone is being prepared, that there could be a crack or a break. In general, the implants need to be put in the bone very tightly which creates a lot of stress within the bone. If this happens it would usually be recognised at the time of surgery and fixed, but is could result in an alteration the rehabilitation afterward with a period of limited weight bearing while the bone heals.
Your Recovery at Home
The success of your surgery will depend in large measure on how well you follow your orthopaedic surgeon’s instructions regarding home care during the first few weeks after surgery
Wound Care : You will have a suture beneath your skin and usually a wound glue as a dressing
The wound can be got wet in the shower but should not be soaked in a bath. After about 2-3 weeks the glue will start to peel off and then massage to the wound area with a moisturiser or bio-oil is helpful to soften up the soft tissues.
Diet: Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron supplement, is important to promote proper tissue healing and restore muscle strength. Be sure to drink plenty of fluids.
Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal light activities of daily living within three to six weeks following surgery. Some discomfort with activity, and at night, is common for several weeks.
- You will be given a home exercise programme to follow by the physiotherapists in the hospital
- With a cementless hip replacement it is advisable to use 2 crutches to aid weight bearing for the first 4 weeks
- It is important not to overdo exercise activity in the first 4 weeks – this will make the hip swollen and more painful
- A significant amount of biological activity is going on in the hip in the first 6 weeks after surgery – in particular bone will be bonding to the implant to provide a robust, secure longterm fixation – this process cannot be speeded up.
- Putting too much stress through the hip too early may affect the bonding to the bone and compromise the fixation of the implant and lengthen the overall recovery.
Blood Clot Prevention: Follow your orthopaedic surgeon’s instructions carefully to minimize the potential risk of blood clots which can occur during the first several weeks of your recovery.
Warning signs of possible blood clots include: Pain in your calf and leg, unrelated to your incision. Tenderness or redness of your calf. Swelling of your thigh, calf, ankle or foot.
Warning signs that a blood clot has traveled to your lung include: Shortness of breath. Chest pain, particularly with breathing.
Notify your doctor immediately if you develop any of these signs.
The most common causes of infection following hip replacement surgery are from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections. These bacteria can lodge around your prosthesis.
Following your surgery, you should consider antibiotic cover for surgical procedures and any dental work where there may be a deep infection.
Warning signs of a possible hip replacement infection are:
Persistent fever (higher than 100 degrees orally). Shaking chills. Increasing redness, tenderness, or swelling of the hip wound. Drainage from the hip wound. Increasing hip pain with both activity and rest.
Notify your doctor immediately if you develop any of these signs.
A fall during the first few weeks after surgery can damage your new hip and may result in a need for more surgery. Stairs are a particular hazard until your hip is strong and mobile. You should use a cane, crutches, a walker, or handrails, or have someone help you until you improve your balance, flexibility and strength.
Your surgeon and physical therapist will help you decide what assistive aides will be required following surgery, and when those aides can safely be discontinued.
To assure proper recovery and prevent dislocation of the prosthesis, there will be a few special precautions. Do not cross your legs. You may bend your hips more than a right angle (90 degrees) but it is important that as you do so you should allow the leg to turn outwards and keep your knee outside the line of your shoulder on that side. This keeps the hip joint in a safe position. Use a pillow between your legs at night when sleeping until you are advised by your orthopaedic surgeon that you can remove it. Your surgeon and physical therapist will give you more instructions prior to your discharge from the hospital.
You may feel some numbness in the skin around your incision. You also may feel some stiffness, particularly with excessive bending. These differences often diminish with time and most patients find these are minor compared to the pain and limited function they experienced prior to surgery.
Your new hip may activate metal detectors required for security in airports and some buildings. Tell the security agent about your hip replacement if the alarm is activated. You may ask your orthopaedic surgeon for a card confirming that you have an artificial hip.
Participate in a regular light exercise program to maintain proper strength and mobility of your new hip. Take special precautions to avoid falls and injuries. Individuals who have undergone hip replacement surgery and suffer a fracture may require more surgery. See your orthopaedic surgeon periodically for routine follow-up examinations and X-rays.
Some surgical approaches to the hip allow earlier and more rapid recovery from the hip replacement operation. One such approach – the Direct Anterior Approach – has particular advantages in that it is muscle sparing and avoids cutting of the muscles around the hip and can be performed through a rather small cosmetic incision. This means that there is less discomfort following surgery and a faster recovery back to normal function. Over the longer term, however, there is probably no difference when compared to more conventional techniques.



