Hip Impingement
Femoroacetabular Impingement (FAI)
This is a condition that has been recognised and understood only relatively recently. This has arisen from the observation that some patients, usually males, develop early arthritis in their hips because their hips have a somewhat aspherical shape. Quite commonly, people who have hips with this abnormal shape, start to get symptoms quite early on and a characteristic pattern of symptoms and x-ray signs are now recognised. The importance in the recognition of FAI lies in the fact that appropriate intervention before arthritis develops may well stop this from developing later in life, or at least delay the onset.
Symptoms of FAI
The condition usually becomes apparent in young athletic individuals who start to get pain in the groin and hip area. This is usually activity related and may become bad enough to result in them having to give up sporting activities. Frequently the condition is considered a “groin strain” and often patients undergo courses of physiotherapy to try and address it. Usually, however, it is rather resistant to treatment with physiotherapy and pain frequently recurs.
Signs
Patients may find that certain movements of the hip have become uncomfortable. This is usually flexion of the hip up towards the chest, as in putting on shoes, and frequently there is a restriction in the amount of internal rotation of the hip.
Diagnosis
Powered by
Clinical Graphics
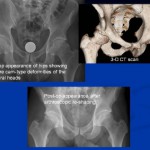
The condition is usually recognisable on plain x-rays of the hip. The hip generally shows an elliptical rather than a spherical femoral head (cam impingement). There may also be abnormalities on the socket side of the hip with too much coverage of the femoral head leading to a different type of impingement (pincer impingement). The signs may be quite subtle and many radiologists who report the x-ray appearance of the hip won’t necessarily recognise the condition. This means that many patients get false reassurance from the report of a normal x-ray when in fact there may be an abnormality present. Once the condition is recognised on x-ray, more investigations may be necessary such as CT scans or an MRI to give more information about the shape of the joint and the damage that may have occurred to the lining of the joint as a result of the abnormal shape.
Treatment
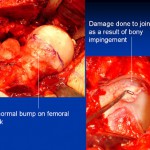
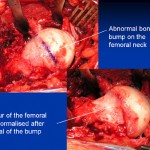
If symptoms cannot be managed by modification of activities, or people find that they can no longer do the activities that they wish, then surgical intervention is appropriate. This involves a procedure to alter the shape of the femoral head and to address the damage that may have occurred to the articular cartilage or lining of the hip joint socket (acetabulum). The aim of the surgery is to improve pain and range of movement in the hip and to try and prevent or halt the progression of arthritis in the joint. This will depend a lot on the amount of damage that may have already occurred and this is very individual from one person to another. Usually it is possible to address the abnormality arthroscopically (keyhole surgery), but open surgery may occasionally be required for specific anatomical abnormalities.
Arthroscopic Treatment of Femoro-acetabular impingement.
The original way in which FAI was treated was through an open procedure to the hip joint (surgical dislocation). Techniques have gradually evolved which make it possible to treat this condition arthroscopically (keyhole approach) This makes a great difference to the speed of recovery from the surgery. Typically the surgery itself may take 1 to 2 hours and is performed under general anaesthetic. Following this, patients start getting out of bed the same day or the day following their operation. Depending on the nature of the surgery to the hip and the findings at the time of surgery the hospital stay is usually only 1 or 2 days.
Rehabilitation following Arthroscopic FAI surgery
The day after surgery, patients start hydrotherapy to work on range of motion exercises to the hip and gentle strengthening. Usually we like patients to use 2 crutches for a period of 2 to 4 weeks (depending on the extent of surgery). After that, the emphasis is on a low impact exercise programme such as using an exercise bike and cross trainer.
Swimming and pool based exercises are also encouraged. This low impact exercise programme continues for 2 to 3 months following the operation. After this period, impact exercises are started such as jogging and gradually built up.
Return to competitive sport is usually 4 – 6 months following surgery.